It’s a given that as we age, we process thoughts a little slower, things may seem a little fuzzier, and we realize that we’ve become more forgetful. Science tells us that this is inevitable. A normal, healthy, aging brain loses its ability to learn and remember, as well as it did in our younger days. Information just doesn’t filter through with the same speed as before. We begin losing cognitive function after approximately the age of 25. Brain cells, like other cells and other organs are dying throughout our entire life, even since birth. It’s a completely natural process called apoptosis.
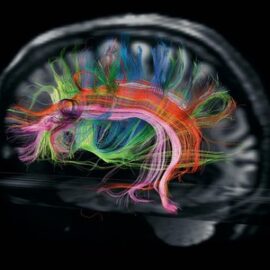
We offset this cellular death in all organs, including the brain, with new cell generation and growth. Brain Stimulating Hormone (BSH) helps generate the growth of progenitor cells, baby brain cells that later develop into functioning neurons. Exercise, incidentally, is the single most important identifiable stimulator of the production of BSH. And there are currently seven BSH identified.
Brain processing speed in particular is one of the many functions that begin to decline after the mid 20s. Maintaining brain processing speed has been identified as one of the most important functions contributing to successful aging. A couple important functions preserved or improved with brain processing speed include frequency of falling and “useful field of vision” that is associated with maintenance of independence. Fear of falling and loss of independence are two of the most important fears voiced by seniors.
But when is this more than just the body’s natural aging process? When does the aging brain turn into something more than just forgetting where you put your car keys or trying to remember your neighbor’s name? Multiple factors contribute to the rate at which brain cells die or lose their connectivity. These can include education, life experiences, genetics, excess alcohol consumption, brain activity after retirement, sleep disorder, stress, depression and anxiety, brain trauma with or without concussion or loss of consciousness, and many other factors.
In the aging brain, manifestations of dysfunction may initially be infrequent, but over time an increase in frequency as well as the type of impairment normally occurs. Very often, acknowledgment of these deficits is made 1, 2 or more years after the onset.
Some observable impairments can be witnessed in the activities of daily life:
• Inability to follow instructions or steps to complete a daily task
• Forgetting how to drive to familiar locations
• Forgetting the names of close family members
• Forgetting appointments
• Inability to complete important tasks like managing a checkbook, or keeping track of important papers
• Forgetting to take medications
• Depression, anxiety, panic attacks
• Sleeping too much or too little
• Not wanting to leave the house, or not wanting company
These behaviors can be a good indication of mild to moderate cognitive decline and impairment that goes beyond simply the natural aging process. Early dementia, effects from chemotherapy, stroke-related impairment, traumatic injury, autoimmune diseases, and more can negatively impact a person’s cognitive ability.
But can there really be something done about it? There’s been a lot of media coverage lately about “brain training” and professional athletes. The National Institute on Aging (NIA) has recently reported in a meta analysis finding 13 treatments worthy of consideration. At the top of the list is computer based training. Unfortunately, they have included only 9 of the over 250 studies published and peer reviewed from academic institutions, and in doing so are minimizing scientifically validated benefit.
However, Neurocognitive Rehabilitation is starting to cause the real buzz. That’s because it encompasses more than just brain training exercises. Advanced clinical techniques combined with unique, medically-proven brain exercises guided by trained brain fitness coaches is just part of a holistic, multidisciplinary approach. The trend is to treat the whole person, not just the brain. Its success lies in the ability to tailor Neurocognitive rehab protocols to each patient. It includes changing a patient’s diet and eating habits, managing their mental health, getting them out of the house, socializing and moving around, helping them with an exercise routine, and ensuring that they are engaging themselves in fun activities and being social – all of these components work together. It’s an effort to help maximize independence and get back some of the brain function that has been lost.
While there is no magic pill, and we certainly cannot turn back time, there are real ways to improve memory, focus and overall cognitive ability, keep your independence and start enjoying life again.